Male hypogonadism refers to a medical condition where the body does not produce adequate testosterone. This is a hormone that plays a critical role in masculine growth and development during teen years at the time of puberty. Impairment in the ability to produce sperms may also be impacted. Not only can a person be born with male hypogonadism, but it can also be developed later in life. Male hypogonadism can be the result of injury or infection as well, besides genetic factors. It all depends on the factors at play and the point at which this disorder occurs. Certain types of male hypogonadism can be cured with testosterone replacement therapy. Before proceeding to the symptomatology and treatment, let’s understand what this disorder is.
Know More About Male Hypogonadism
Table of Contents
Specifically, testosterone is commonly associated with masculine growth during puberty and sperm production. It is a steroidal hormone that decreases in volume in patients who suffer from male hypogonadism. This is a disorder in which the testes fail to produce a sufficient amount of the hormone. One or both testes may be affected. While male hypogonadism is noted in elderly patients, on account of increasing age, factors like infection and injuries also result. In certain specific cases, male hypogonadism has even been found to occur in children since birth. Symptoms and effects showing up will depend on the cause and age at which the disorder manifests itself.
The Symptoms
Photo by: OpenStax College/CC BYThe stages at which male hypogonadism can occur are divided into adulthood, pre-teens and fetal. Fetal development of male hypogonadism means the body produces insufficient testosterone hormone at the time the fetus is developing. In such cases, a genetically masculine child may suffer from any of the following:
- Have underdeveloped genitals
- Have certain female genital features
- Have genitals that are neither male or female, but uncertain
If it occurs before puberty, male hypogonadism can lead to abnormal development and cause the following:
- Less masculine or deep voice
- Abnormal testes and penile growth
- Abnormal amounts of body hair
- Development of breast tissue or gynecomastia
- Insufficient muscle mass development
- Abnormal arms and legs growth
During adulthood, hypogonadism damages reproductive function and symptoms range across the following:
- Low muscle mass
- Development of gynecomastia
- Declining bone mass or osteoporosis
- Infertility
- Erectile problems like dysfunction
- Abnormal body and facial hair growth.
At this time, due to following testosterone levels, victims may suffer from the following symptoms:
- Difficulty in concentrating
- Fatigue and tiredness
- Failing sex drive
- Hot flashes
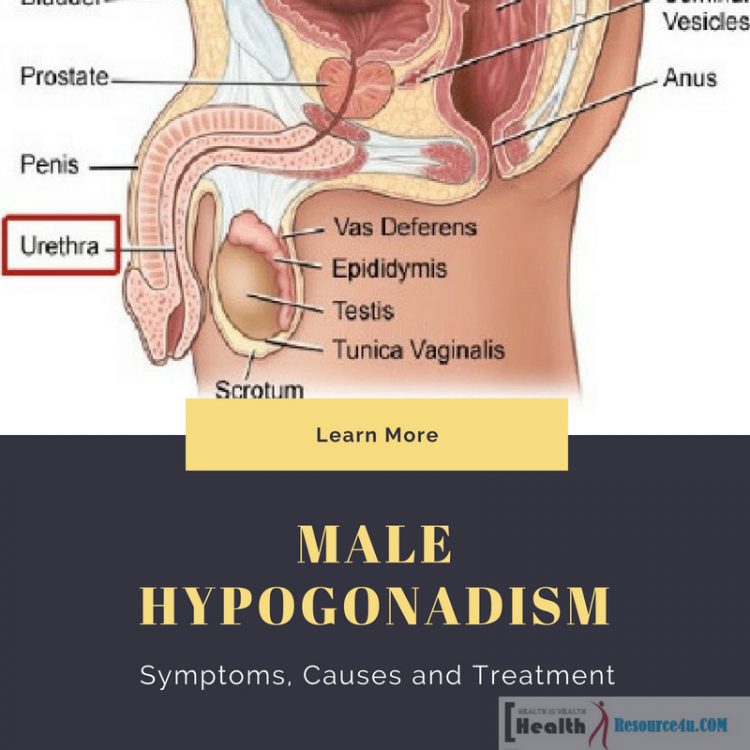
The male reproductive system stores make and move sperm. The production of sperms takes place in the testicles. Fluid from the prostate gland and seminal vesicles unite with sperm to produce semen released from the penis during sexual intercourse.
For those having symptoms of male hypogonadism, establishing the cause is the most important first step to getting the required treatment. As male hypogonadism is a form of testosterone deficiency, it results from the inability of the testes to produce that specific hormone, and in some cases even sperm. Specifically, the condition can result from testicular disorders or be the result of disease processes influencing the hypothalamus and pituitary gland.
Male hypogonadism can impact different organ functions and impact the quality of life. Signs and symptoms are entirely dependent on when the disorder started, how severe the deficiency is and whether there is an impairment in the functionality of the testes. Hypogonadism’s impact is based on when it starts. If male hypogonadism takes place prior to teen puberty, developmental changes associated with puberty do not progress. For those facing this disorder post-puberty, there is infertility and sexual dysfunction.
In adult men, symptoms commence within a few weeks of the onset of this deficiency or shortage of testosterone. This disorder also raises the chances of contracting type 2 diabetes or suffering from cardiovascular disorders, metabolic syndromes, or even premature death in older men and Alzheimer’s disease.
In cases where adults develop male hypogonadism, erectile dysfunction is a major symptom. Lack of this hormone testosterone can also influence the onset of other symptoms which depend on the age at which the disorder develops and the degree of testosterone deficiency. Also equally important is the period of time for which testosterone function has been adversely impacted.
For teens and young adults who have not completed puberty, the disorder can make them look younger than their biological age. They also suffer from small genital size, lack of bodily and facial hair and failure of the voice to become deeper. They also experience difficulty in gaining muscle mass, even with exercise. Male hypogonadism at the onset of puberty can lead to the impairment of sexual development, diminished testicular size and enlargement of the breasts or female characteristics.
Adult-onset male hypogonadism is also associated with erectile dysfunction, low sperm count, decreased libidinal strength and depression. Some mental symptoms are also noted such as loss of sleep and a sense of listlessness and lethargy. Loss of body hair such as facial, axillary and private regions, can also be a problem. Apart from enlargement, there is also discomfort in the breast region. Hot flashes, increased body fat and sweating are some physical sensations. Apart from this, energy and concentration levels dip too.
Causes
Hypogonadism results from decreased functional activity within the gonads. For males, the gonads are the testes, while for females, they are the ovaries. The gonads secrete hormones and gametes which are egg or sperm. A wide number of hormones are released by the gonads. These include testosterone, antimullerian hormone, inhibin B, progesterone, estradiol, and activin. Male hypogonadism specifically results when one or both testes fail to produce enough testosterone. This is a hormone which plays a critical role in sexual, as well as cognitive and body functions and development. Low testosterone levels also lead to the absence of secondary sex characteristics apart from the lack of muscles, or increased muscle wasting and lack of fertility. Other abnormalities and pathologies may also be noted. Low levels of testosterone can result from testicular, pituitary or hypothalamic pathologies or abnormalities. In those who present clinical symptoms and signs, guidelines are needed for treating the disorder. Mostly, treatment of the condition involves testosterone replacement.
Different Types and Etiology/Causes
There are two basic types of male hypogonadism namely primary and secondary.
Primary Hypogonadism
This is called primary testicular failure and takes place from a problem in the testicles.
Secondary Hypogonadism
This type of hypogonadism occurs when there is a problem in the pituitary gland or hypothalamus. These are the brain parts that signal the testicles to produce testosterone. The hypothalamus produces the hormone which stimulates the gonads and in turn, which signals the pituitary gland to make hormones like LH and FSH. The luteinizing hormone serves as an important signal to the testes to secrete testosterone. Any of these types of hypogonadism can be caused by inherited or birth trait and
Causes of Primary Hypogonadism
#1 Klinefelter’s Syndrome
Photo By: Xasodfuih/ CC BYThis is a syndrome that results from a birth defect of the sex chromosomes X and Y. A male generally has one X and one Y chromosome. In this syndrome, two or greater number of X chromosomes are present along with the single Y chromosome. This Y chromosome contains a genetic material that determines the child’s sex and gender-related development. The additional X chromosome(s) in the syndrome cause abnormality in the development of testicles and underproduction of testosterone.
#2 Undescended Testicles
Prior to birth, testicles remain inside the abs and move down to their permanent spot on the scrotum. However, there may be a problem in that one or both testicles fail to descend at birth. This condition often is self-correcting within the first few years of life sans treatment. However, in case it is not corrected in early childhood, it leads to malfunction of the testicles and reduced testosterone production.
#3 Mumps Orchitis
In case a mumps infection concerns the salivary glands as well as the testicles, it is known as mumps orchitis. This condition occurs during adolescence or adulthood. It is characterized by long-term damage to the testicles. This impacts normal testicular functioning and testosterone production.
#4 Hemochromatosis
This is a condition which results when there is excessive iron in the blood. This leads to testicular or pituitary gland issues. This also impacts testosterone production. On account of its location external to the abs, the testicles are prone to serious injury. Damage to normally developing testicles such as injury to one or both may cause this disorder too.
#5 Treatment of Cancer
When chemo or radiation therapy is used for the treatment of cancer, it can obstruct the effective functioning of testosterone and sperm production. The impact of these treatments are short term, but the result can be long-term or irreversible damage to fertility. Once the treatment ends, men may recover their fertility after a few months, but this is not always possible. Preserving sperm before commencing cancer therapy is an option many people do consider/ Research has shown 30% of males with cancer and 90% with germinal epithelial dysfunction suffer from male hypogonadism.
#6 Normal Aging
Older men have lower levels of testosterone as compared to younger men. As men become older, there is a slow and continuous decrease in testosterone production. The rate of decline of testosterone varies across men. Close to 30% of men older than 75 years of age have below normal levels of testosterone, according to research by the American Clinical Endocrinologists Association. Whether the treatment is necessary or not remains a question of debate.
Causes of Secondary Hypogonadism
In the case of secondary hypogonadism, testicles are normal but the function is impaired on account of issues with the hypothalamus or pituitary. Numerous conditions lead to this form of hypogonadism as detailed below.
#1 Kallmann Syndrome
Abnormal hypothalamic development can also lead to hypogonadism. This is essentially the area of the brain that controls the secretion of pituitary hormones. In Kallmann syndrome, this type of pathology is noted. It also leads to problems in the ability to smell or anosmia.
#2 Pituitary Disorders
Abnormalities in the pituitary gland impair hormone release from the gland to the testicles. This adversely impacts testosterone production. A brain tumor like a pituitary tumor located near the gland may also lead to hormonal deficits and testosterone deficiency. The treatment for a brain tumor like radiation or surgery can impact pituitary function and lead to hypogonadism too.
#3 Inflammatory Diseases
Certain diseases which lead to inflammation such as tuberculosis, histiocytosis, and sarcoidosis involving the hypothalamus and pituitary gland can impact testosterone production, leading to hypogonadism.
#4 AIDS-HIV
This virus leads to low levels of testosterone affected by the hypothalamus, pituitary, and testes.
#5 Medications
Use of specific medicines such as opiate pain medications and hormonal treatments can initiate lower hormone production and less testosterone in the body.
#6 Obesity
Obesity and overweight tendencies are linked to lower testosterone.
#7 Stress Induced Hypogonadism
Stress, too much physical activity, and weight loss have all been linked with hypogonadism. This has also been attributed to stress-induced hypercortisolism, suppressing the hypothalamic functioning.
Link with Testosterone Deficiency
Across the male lifespan, testosterone plays an important role in cognitive, sexual and body development. At the time of fetal development, testosterone helps in sex determination. Most visible impact of rising testosterone levels commences at the pre-pubertal stage. At this time, body odor may emanate, even as oily skin and hair result in the development of acne, and growth spurts along with body and facial hair. Even as adults, effects of testosterone are visible in the form of aggression, libidinal disturbances, erectile dysfunction and variances in energy levels.
How the Brain Influences the Disorder
The gray matter or the cerebral cortex is the brain’s layer which is its most highly developed portion. This is the part of the brain covering 2/3rd of the brain mass. It carries out complex information processing in the brain. Within the portion of this brain, the production of hormone testosterone commences. The cerebral cortex signals the hypothalamus to stimulate testosterone production. For this, the hypothalamus secretes the gonadotropin-releasing hormone in a pulsatile fashion. This, in turn, leads to the stimulation of the pituitary gland- the brain’s portion involved in regulating growth, blood pressure, thyroid function and other key functions of the body. Once the gonadotropin-releasing hormone stimulates it, the luteinizing hormone triggers activities in a certain class of cells in the male testes known as Leydig cells. These cells are central to converting cholesterol to testosterone. When testosterone levels are adequate, the pituitary gland slows the LH or luteinizing hormone through a feedback mechanism that is negative. This slows down testosterone production. This is implicated in low testosterone levels. Changes in testicles, pituitary gland or hypothalamus can result in hypogonadism. Such differences can be acquired or congenital, permanent or temporary.
Recent research has found that testosterone levels are decreasing slowly due to age. The rate of decline varies. Unlike cases where the hormone levels in women face a rapid decline at the time of menopause, men experience the decline over a gradual, slow period of time. In one longitudinal study conducted in Baltimore, close to 20% of men in their 60s and half of the men in their 80s are hypogonadal. A New Mexico study found a decrease in serum testosterone of 110 ng/dl every decade. As hormone levels slowly decline, this hypogonadism is known as partial androgen deficiency of the aging male.
Obesity and Its Linkage to Hypogonadism
Photo by: CDC/CC BYIrrespective of comorbid conditions or age, obesity is linked to hypogonadism. Reduced testosterone levels are found in men with more abdominal adiposity. Proposed causes for the impact of obesity on testosterone levels include aromatization or clearance of testosterone in the fatty tissues and increased inflammatory cytokines, decreasing the secretion of gonadotropin-releasing hormone. Alike the projections for older men, obese and overweight men may also be prone to hypogonadism. When risk factors of age and obesity are removed, diabetes remains another lifestyle disease implicated in the etiology of hypogonadism. Certain medicines like corticosteroids, ethanol, opiates, psychotropic medicines, and ketoconazole are also associated with low testosterone
Testing and Treatment
Early diagnosis and treatment can lower risks associated with hypogonadism. Quick and early detection in young boys can ward off problems on account of delayed puberty. Early diagnosis in men protects against the development of conditions like bone loss. Diagnosis is based on blood work and assessing symptoms, especially on testosterone levels. The first step towards diagnosis is the Androgen Deficiency in Aging Male testing. This questionnaire identifies men who exhibit signs of low testosterone. Testosterone levels change across the day and are highest in the morning period. If testosterone levels are low, the tests to detect this range across semen analysis, hormone testing, pituitary testing, genetic studies, and testicular biopsy. Once the treatment commences, the patient can continue to have testosterone levels to assess if the medication is producing adequate testosterone levels.
Male hypogonadism is associated with a fall in one or both of the testes’ key functions namely testosterone hormone and sperm production.
Doctors also conduct physical exams to confirm sexual development at the right level for the right age. Muscle mass, body hair and sex organs are also examined.
Hormone Testing
When it comes to hypogonadism, the testing involves checking sex hormone levels. Blood tests can be checked to assess levels of follicle stimulating hormone and luteinizing hormone. The pituitary glands are secreting this reproductive hormone. Testosterone is drawn for testing in the morning when hormone levels are highest. If one is male semen analysis will also be conducted to check the sperm count.
Doctors can order blood tests to confirm male hypogonadism and rule out underlying causes. Additionally, levels of iron in the blood impact these hormones. Thyroid testing is also mandatory as it can trigger symptoms similar to hypogonadism.
Imaging
Tests for imaging can also prove useful for diagnosis. Ultrasounds and MRI scans can be used.
Testosterone Replacement Therapy
Male sex hormone testosterone is lowered in this disorder. So testosterone replacement therapy is widely used for warding off male hypogonadism. Testosterone replacement therapy can be administered through gel lozenge, patch or injection works well. Injections of this gonadotropin-releasing hormone trigger puberty or raise sperm production.
Testosterone replacement therapy is a primary treatment for male hypogonadism. Therapies need to provide physiological testosterone levels. Guidelines from the American Association of Clinical Endocrinologists indicate sexual function is restored, and there is the protection of libido, behavior and well being. It also enhances and maintains virility. It also prevents osteoporosis and optimizes the density of the bone. In aged seniors, TRT can normalize growth hormone levels. It impacts the cardiovascular disease risk. In cases of hypogonadism, fertility is restored when it is hypogonadotropic.
Transdermal testosterone patches are under the brand name Androderm. These patches deliver constant testosterone over a 24-hour period. Application site reactions are some adverse side effects. Skin irritation may result along with local reactions like pruritis, erythema, vesicle formation, blistering under the patch, indurations plus allergic contact dermatitis. Close to 10 percent of the patients discontinue patch therapy due to skin irritation.
Topical testosterone gels are also available. The application allows testosterone concentrations to follow the correct circadian patterns, in this context. Testosterone through gels does not undergo the first-pass metabolism. It can lead to increased blood pressure acne, headache, and hot flushes as well as emotional lability and anxiety. Skin irritation is less with gels.
Buccal testosterone tablets, release testosterone in a pulsatile manner. It is akin to an endogenous secretion. The peak testosterone levels are attained quickly and lasting results follow. Buccal administration avoids the first-pass metabolism. Drug absorption is not altered by food and beverage. Transient gum irritation and bitter flavor are some of the adverse effects.
An implanted pellet releases testosterone through zero order kinetics across the months. Peak testosterone levels can be attained within half an hour. Some problems with this method of TRT is minor bleeding, fibrosis, and pellet extrusion.
Intramuscular injections are also beneficial. Peak levels take place within 72 hours of administration. Post-administration, high testosterone levels are achieved. For preventing fluctuations, shorter dosing periods and lower doses may be recommended. Despite fluctuations in testosterone, intramuscular injections can prove to be a cost-effective option.
Testosterone is generally not taken orally because multiple daily doses are required. Additionally, oral products show elevated liver enzyme levels, acne, GI intolerance, and gynecomastia.
Long-Term Outlook
As per research, hypogonadism is a chronic condition requiring lifelong, long-term treatment. The testosterone hormone decreases if treatment is stopped. Support through therapy can help before, after and at the time of treatment. Testosterone replacement therapy also improves the mood and quality of life in males with this disorder. TRT is the recommended treatment for this. Given through topical gel, injection or transdermal patch, testosterone is generally not administered in oral form.
Benefits of TRT include an increase in libido, mood improvement, enhanced bone mineral density and improved quality of life. Some risks were associated with it. It leads to worsening of heart, prostate cancer, sleep apnea, and BPH conditions, where it cannot be administered without attending to conditions.
Males undergoing TRT require ongoing medical evaluation to determine the appropriate treatment response. This includes frequently conducted blood tests and periodic digital rectal examination. TRT is also contraindicated in those with erythrocytosis, where there is a high volume of RBC in the blood. Responses to TRT are individual and personalized. It should be noted that testosterone levels are not an indicator of who responds to TRT and who does not. While it can relieve male hypogonadism symptoms, TRT does not increase fertility.
Lifestyle Changes
Certain lifestyle changes can boost testosterone levels including weight loss, regular exercise, adequate sleep and elimination of smoking. These measures help in the maintenance of normal testosterone levels.
A thorough medical history is carried out when hypogonadism is at risk. Serum total and free testosterone blood tests are conducted. Only readings between 1000 and 300 ng/dl are considered healthy. Levels below this range are noted with those with hypogonadism.
The blood test should be drawn on two occasions between 7 and 11 am in the morning. Additional testing is needed for confirming male hypogonadism.
Final Word
Hypogonadism impacts men of different ages through acquired or birth causes. For those who have clinical symptoms associated with low levels of testosterone, treatment is essential for preventing bodily, mental and sexual changes. Numerous treatment options are available, using different dosage formulations and providing choices that best meet needs. Hypogonadism is a clinical condition with a lot of consequences. Prompt treatment is essential to prevent further complications.