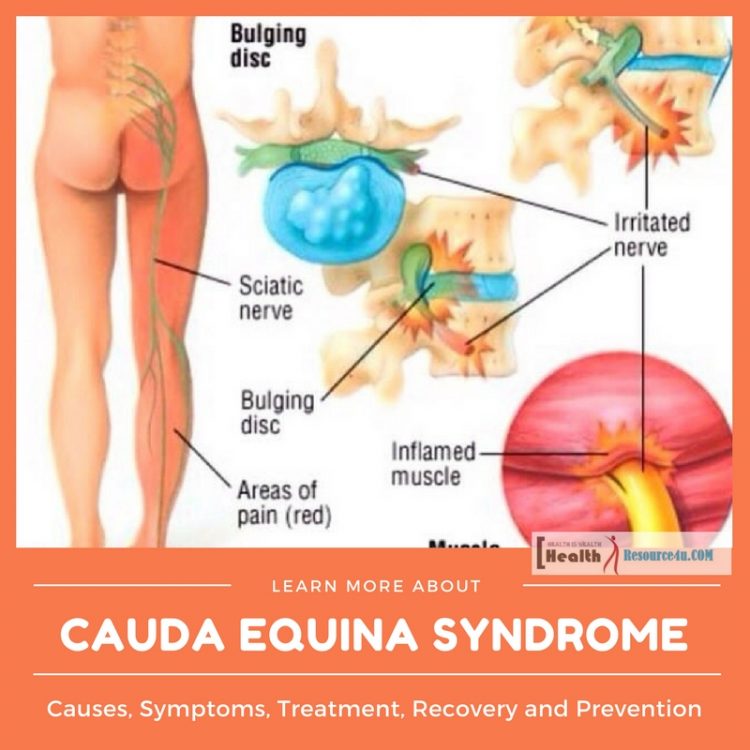
Cauda Equina syndrome sounds like a complicated disease. It is actually quite a complex one. The syndrome results from the complication of nerve compression at the spinal cord base within the spinal canal. This is caused by a condition that results in pinching or irritation of the nerves at the spinal cord end. The main symptoms of this syndrome center around pain. There’s a general pain in the lower back, numbness or tingling in the lower extremities and glutes or sciatica and incontinence as well as legs weakness. This syndrome is diagnosed in relation to certain symptoms and confirmed by neurologic and radiology testing. This is a medical emergency with the need for a surgical decompression operation. The neurological or nerve tissue damage determines the prognosis and outlook for patients.
Cauda equina stands for the tail of the horse. It is a reference to the usual anatomy at the close of the spinal cord in the lower back, where it divides into nerve tracts akin to the tail of the horse. The spinal cord compression at this point can lead to the different symptoms of this syndrome. These include lower backache, sciatica, bladder and bowel incontinence, saddle sensory changes and lower extremity sensory and motor loss.
The lower back pain is the most common symptom, affecting millions of people. In many cases, surgery is not required for curing low back pain. But in case it is a sign of this syndrome, the severe back pain is a condition that requires surgical treatment. Individuals with cauda equina syndrome often get to the emergency ward of the hospital, because of the excruciating pain.
In patients with this syndrome, there is compression on the spinal nerve root. Faster treatment may be required to prevent damage caused by incontinence and paralysis set in the legs. This syndrome affects the roots of the nerve called cauda equina or the horse’s tail in Latin. The affected nerves are located at the spinal cord’s lower end in the lumbosacral spine. Messages are sent and received from the feet, legs and pelvic region. Because of this syndrome, the spinal cord nerves at the base undergo compression. This impacts nerves critical for leg, feet and pelvic organ massage. This is a complicated medical condition which can trigger back problems, lower back pain, paralysis as well as problems of incontinence.
Cauda equina syndrome requires treatment at the hospital emergency medical ward to avert serious problems.
Causes
Table of Contents
This syndrome occurs in grown individuals rather than children. It can also take place in children with spinal injury or spinal birth defect. The most common causes of Cauda Equina Syndrome are as followed. The most well known and commonly occurring cause is a lumbar area ruptured disk. Additionally, the spinal canal narrowing, also called stenosis also causes this condition. The spinal infection, hemorrhage, inflammation or fracture can also be the cause of this disorder. Trauma to the lumbar spine from car crashes, stabbing, gunshot wounds or falls can also be the cause of this syndrome. Birth defects such as abnormal linkages between blood vessels or arteriovenous malformation are yet another cause.
Cauda equina syndrome is caused by conditions that result in pinching of the nerves or direct irritation. This syndrome also results from lumbar intervertebral disc herniation. It can also be the consequence of tumor or cancer-causing abnormal growth next to the lower spinal cord. There’s also a localized infection close to the spinal cord, resulting in localized bleeding or epidural abscess or hematoma, leading to pressure on the lower back and pain in the spinal cord.
Localized lumbar tumors can cause CES including ependymomas, Paget’s disease of the bone and metastatic cancer. Spinal cord’s localized infections can be the result of staph bacterial infection or tuberculosis bacteria caused by Mycobacterium TB from Pott’s disease and many others. Nerve compression associated with CES is causing the lumbar herniated disc. Lumbar discs can lead to single injury linked herniation especially when excessive pressure is exerted on the lower portion of the spine. It can also take place when there is rupture or straining of the weakened disc.
Herniated Disc
Generally, a herniated disc does not impact the cauda equina part of the spinal cord. CES resulting from lumbar disc issues requiring surgery range from 2-6 percent of the entire cases. A lot of disk herniations are self-limiting and improve independently. These also respond to anti-inflammatory medicines, physiotherapy and short rest periods. CES can result from herniated lumbar disk, occurring mostly at the following vertebral levels- L4-L5 or L5-S1. A large percentage of 70% of the herniated disk cases lead to CES in those with a chance of developing chronic or long-standing lower back pain. Some develop cauda equina syndrome as the first symptom of lumbar disk herniation. Those in their 30s and 40s are more prone to CES by disk herniation. Many cases of cauda equina syndrome involve larger particles of disk material completely separated from the normal disk and compress the nerves or extruded disk herniations. In a lot of cases, disk material takes up 1/3rd of the canal diameter.
Other Causes
Along with lumbar herniated disc, other factors may also lead to CES.
Lumbar spinal stenosis is when there is pressure on the spinal canal, resulting in CES. Inflammatory conditions can lead to CES if inflamed tissues or bony overgrowth can press on the lumbar nerve roots. An example of this condition which leads to CES syndrome is ankylosing spondylitis. Spinal canal infections such as osteomyelitis or spinal epidural abscess press into the spinal canal, resulting in neurological symptoms.
Photo by: Page TFW/ CC BYTumors or neoplasmic growth near the spine can also place pressure on the spinal canal. These tumors occur in the spine but are caused by cancer becoming malignant and spreading from other parts of the body towards the spine. Trauma such as car accidents or falls or penetrative injuries can also cause CES and produce neurological symptoms.
Post-operative complications from lumbar surgery are experienced in those with CES post surgery for repairing the lumbar herniated discs.
Risks associated with CES are the same as those leading to spinal stenosis and lumbar herniated discs. This includes overall lifestyle and health, such as ingestion of alcohol, smoking, low levels of activity and obesity. Other trigger factors include being between 50 to 30 years of age and opting for work that is labor intensive.
CES develops more often in adults than kids. It can occur in children with a spinal birth defect or spinal injury. Common causes of CES include:
- Herniation or bulging of lumbar area spinal disks that press on nerves.
- Spinal cord narrowing or stenosis.
- Spinal tumor or lesion.
- Spinal cord, infection, fracture, hemorrhage.
- Complications from trauma to the lumbar spine
- Birth defects resulting in abnormally connecting blood vessels.
CES is caused by considerable narrowing of the spinal canal that compresses nerve roots below the spinal cord level. Many causes of cauda equina syndrome include traumatic injury, spinal stenosis, disk herniation, spinal tumors or neoplasms like metastatic tumors, schwannomas, ependymomas, meningiomas, infectious and inflammatory conditions. causes by medical intervention or iatrogenic causes.
Trauma
Traumatic events lead to subluxation or fracture/partial dislocation of the lumbar spinal region or the lower back. This results in cauda equina syndrome. Another reason for compressing the cauda equina is the collection of blood surrounding the nerves post the trauma or epidural hematoma in the lower back. Any penetrating trauma like stab wounds or gunshots can lead to damage/compression of the cauda equina. Rare spinal manipulation complication also results in subluxation of the lower back or lumbar spine, leading to CES.
Spinal Stenosis
This refers to the narrowing of the distance of the normal front to back of the spinal canal. Spinal canal narrowing can lead to degeneration or developmental abnormalities. The abnormal forward slip caused by one over another vertebral body is known as spondylolisthesis. Certain cases can lead to spinal cord narrowing and lead to the development of CES,
Neoplasms/Tumor
Photo by: Henry Vandyke Carter/ CC BYCES is also the result of isolated or primary neoplasms or tumors. The tumor may also spread from the spine to other body parts such as metastatic spinal neoplasm. These tumors are commonly the metastasizing from lung or prostate in men and from lung and breast in women. A common starting system of CES caused by spinal neoplasm is severe lower back and leg pain. Sensory loss/loss of leg feeling and lack of bladder or bowel control are common.
Inflammation
Chronic spine inflammatory conditions include ankylosing spondylitis and Paget’s disease, leading to spinal canal narrowing and causing CES.
Infection
Spinal canal infections or spinal epidural abscesses can lead to the spinal column and nerve root deformity. Symptoms range across severe back pain and increasing muscle weakness.
Accidental Medical Reasons/Iatrogenic Causes
Ill positioned screws on the spinal cord can lead to compression and nerve injury, resulting in the development of this syndrome. Constant spinal anesthesia has been associated with CES too. Lumbar puncture or spinal tap can lead to blood aggregation in the spinal canal causing spinal epidural hematoma in spontaneous form, in those getting anticoagulants or blood thinning medication. Collection of blood leads to nerve compression and development of the cauda equina syndrome.
Back pain is a complaint which is common, but it can be triggered suddenly and includes numbness in the genital section, a problem in urination and legs weakness. It can lead to a medical emergency. Cauda equina syndrome leading to large disc herniation in the lower back leads to nerve root compression at the spinal cord end. These nerves transmit messages from and to bladder, legs, and bowel. If there is pressure on them for long, damage can be irrevocable. Quick surgery to prevent pressure can lead to permanent damage and restoration of bowel and bladder function.
Symptoms of Cauda Equina Syndrome
The cauda equina is a spinal nerve bundle located in the lumbar spine or lower back. Branches emanating from the nerves reach the pelvic organs, colon, and bladder. Nerves continue through the pelvis and down the back of the leg in the form of sciatic nerves. CES is a rare condition with detrimental consequences if it is not properly treated. Nerves are bundled together, resembling the horse’s tail, after which this name in Latin is derived.
Unlike other chronic back problems, CES is an acute condition like a heart attack or stroke. It often emerges rapidly, with just six to ten hours for manifesting. Classic back pain symptoms online with sudden numbness onset in the genital area and abrupt urine retention are indications of an emergency. Relief of compression rapidly determines whether one lives normally or suffers paralysis in the legs and incontinence. In those with recurrent back problems, CES has a gradual onset.
In those with recurrent back issues, cauda equina syndrome comes on slowly, with gradual symptom progression, because CES is a nerve disorder that leads to bladder control loss. The symptoms can be akin to those exacerbated by prostate or bladder problems. A massive ruptured disc leads to CES. At the time of herniation, the center which is gel-like can cause the bulging or rupture of the spinal disc, through weak areas in the wall leading to nerve compression. In a lot of cases, disc herniation occurs between the L5-SI or L4-S lumbar spine discs. Falls, car accidents or sports injuries can lead to spinal fracture, muscle tear, or damaged nerves. Other causes can be spinal cord narrowing, hemorrhage, infection or tumor.
Diagnosing CES can be tough. Symptoms differ and may have a gradual onset. They also replicate other medical conditions. These are the symptoms of CES:
- There may be severe pain in the lower back.
- Additionally, pain, weakness or numbness in a single or both legs can cause a person to stumble or have problems getting up.
- Loss of or changes in sensations in inner thighs, leg backs, legs, glutes or feet may occur. There may be severity and the condition may worsen.
- Along with this, there may be trouble in areas of the body sitting in the saddle (known as saddle anesthesia too).
- There may also be problems with bladder or bowel functioning such as difficulty in urine elimination or waste removal.
- Retention or incontinence may result.
- Sudden onset of sexual dysfunction may also take place.
- CES also includes tingling and pain in back and lower extremities also called sciatica,
- Legs weakness and bladder or bowel incontinence can be another problem.
- CES is associated with numbness in different parts of the body too.
When there is partial compression of lower spinal cord nerves, partial CES is diagnosed. This can cause numerous degrees and combinations of different symptomatology. With the complete version of the syndrome, the common symptoms manifest more regularly. Additionally, leg weakness, pain or numbness can cause trouble in movement. The pain can be searing and get worse. Pain may also travel through the thigh, past the knee to the foot and calf.
Treatment of Cauda Equina Syndrome
Diagnosis
A medical professional diagnoses this syndrome through the following measures:
- Medical history: Here the patient provides data about activity levels, symptoms and health.
- Physical exam: This assesses reflexes, strength, sensation, stability, motion, and alignment. Blood tests may also be needed.
- MRI scan uses magnetic fields and computers to produce 3D spinal images.
- Additionally, a myelogram or an X-ray of the spinal canal post the injection of contrast material can pinpoint the source of pressure on nerves or spinal cords.
- A computerized tomography or CT scan.
CES is clinically diagnosed based on certain symptoms and physical exams can indicate lower extremity based hyperactive reflexes. As the syndrome triggers a medical emergency, spinal surgery consultants or neurosurgeons should be immediately notified. CES can be confirmed with radiology and neurologic testing and it should not be delayed.
Specialized nerve testing of the lower body parts can also take place. This includes nerve conduction velocity and electromyography tests that indicate nerve irritation effects in the lower back. CT or MRI are other forms of radiologic testing that lead to spinal cord tissue compression monitoring.
CES is a medical emergency, with spinal nerves compression of the spinal cord triggering a permanent incontinence or retention problem. Once this syndrome is diagnosed, treatment including aggressive interventions and surgery aimed at decompression take place. In case the infection is prevalent, antibiotics are intravenously administered. In case the tumor is causing compression, chemo, radiation therapy or surgical decompression may be needed.
Long-term CES management is based on whether or not there are consistent symptoms post-surgical decompression of the irritated nerve tissue. This leads to physical therapy problems, pain medicine, supportive braces, urinary catheters, and several other treatments, This occurs until the nerve and muscles recover their normal state.
MRI is the normal way to confirm the CES prevalence, and the sooner the syndrome can be diagnosed, the better the chances of sound recovery and experience occur, a few symptoms of nerve damage may continue to have lingering impact otherwise. For patients with acute CES, surgery is an urgent need. The aim is to provide relief on the spinal nerves for restoring sensation and functioning to the legs, bowel, and bladder.
Surgery
Based on the cause of the syndrome, the following surgical operations may be performed:
Discectomy for herniated disc leading to the removal of disc portion associated with nerve compression. Surgeons make tiny incisions in the middle of the back. Spinal muscles are moved on one side to expose the vertebra’s bony section. A bone window is removed to reveal the disc and nerve root. The portion of the disc which is ruptured for compressing the spinal nerves is removed carefully. Spinal decompression for stenosis also removes the spurs of the bone and ligaments implicated in nerve compression. This involves the creation of a tiny incision in the back The bone is removed from the spinal canal roof. Soft tissues, as well as bone spurs, are removed to create additional room for the nerves. Lesions such as tumors can also be removed. Clinical trials are research studies in which diagnostics, procedures, fresh treatments, and other therapies are tested to check if these are safe and effective. Research is also conducted to improve medical care standards. Information about present clinical trials can be found online. Studies are being conducted not just by government bodies like NIH, but also pharmaceutical companies and the private industry.
Surgical procedures need to be rapidly carried out to prevent loss of control, resulting in paralysis or other linked problems. Surgery needs to take place within 48 hours of symptoms onset. Based on the CES cause, high doses of corticosteroids may also be needed. This can reduce inflammation. If an infection is diagnosed, antibiotics may be needed. If tumors are the cause, radio or chemotherapy may be needed post surgery.
Even post the treatment, full functionality may not be recovered. It all depends on the extent of the damage. For those with successful surgeries, bladder and bowel function may continue over the years.
CES takes place as a result of conditions that are unpredictable make this a nonpreventable syndrome. However, CES by an infection caused by IV drug addiction can be prevented by working on nonuse of drugs.
CES requires surgical decompression to decrease or cut down on the pressure in the affected nerves. Surgeons opine that decompression needs to be carried out as quickly as can be, within lesser than about 8 hours since the sudden onset of symptomatology. Using a surgery known as lumbar laminectomy, CES is often treated.
Surgery within a day to two days of the onset of symptoms offers a chance for maximum recovery and improvement of any sensory-motor deficits. Patients undergoing surgery within around 48 hours since onset the symptoms were discovered to have a better prognosis as opposed to those operated beyond this time limit. Patients who have surgery may experience improved bladder and bowel control and overcome neurologic deficits.
While lumbar laminectomy may be the best cure, lumbar microdiscectomy can also be performed. Patients will be staying at the hospital for some days to monitor recovery of sensory and motor functions.
Prognosis Post Surgery
Prognosis for CES is based on numerous factor or aspects, such as the speed at which nerves are decompressed and extent of nerve damage at surgery. Post surgery, the recovery varies, depending on a lot of factors. Patients may experience lower-back and/or leg pain, bladder/bowel problems and other physical issues based on the extent of compression of the nerves and symptom severity during surgery.
Though it is usually perceived that CES linked neural damage is permanent, certain studies indicate longer-term management may permit patients with poor prognosis post surgery to get back to near normal bladder movements with less interruption. Medical treatment options are also useful in specific persons, based on the underlying core of the syndrome. Moreover, anti-inflammatory agents like ibuprofen and corticosteroids can impact people with inflammatory processes such as ankylosing spondylitis. Those with CES resulting from infections should get the right antibiotic therapy. People suffering from neoplasms or spinal tumors need to be evaluated for chemo and radiotherapy.
Care should be taken for medical management of this syndrome. Any person with CES and groin numbness or weakness of legs or loss of bowel and bladder control should ensure medical management within 24 hours of the symptoms. If there is no relief during the period, instant surgical decompression is needed to minimize permanent nerve injury.
Recovery and Prevention
Certain bladder and bowel functions are automatic, but even those under voluntary control can be lost with CES development. This can cause trouble in the elimination of waste from the body and even lead to either incontinence or retention. Recovery is linked to the symptoms severity and the duration of time for which the nerves were compressed prior to performance of surgery. Chance of full recovery for those with urinary retention worsens. Of those who suffer partial CES or numbness/tingling in lower extremities, close to ninety percent will regain normal bowel, bladder, and sexual functioning. Those who suffer complete CES or bladder retention have a lower chance of recovery, with twenty percent suffering from permanent incontinence and sensation loss in pelvic areas.
Remaining problems post the surgery may take months to resolve. Rehab methods like bladder retraining may be needed. People with permanent injury face everyday adjustments in lives, Physiotherapy can serve as a useful method of managing the symptoms. Self-catheter use, stress alleviation, and relaxation techniques need to be in place. Additional help can be provided by medical professionals like sexologists, psychiatrists, social workers or even a support group. Paralysis of the legs may also occur in a few cases.
For treating cauda equina syndrome, prompt therapies are essential to relieve nerve pressure.
Medication for CES
Those with infections or tumors caused by infectious or neoplastic causes resulting in CES need to receive the right antibiotics or chemo for treating the underlying cause. Treatment using medicines alone is not recommended because of the need for release of the nerve compression or surgical decompression of the spinal canal.
Conclusion
Finally, the patient outlook for those suffering from CES is based on the damage caused by nerve tissues. Generally, the longer the spinal cord compression, the greater is the recovery period and complete recovery can take place. Prompt treatment is needed to relieve nerve pressure. Surgery needs to be carried out to prevent permanent damage such as leg paralysis, loss of control or sexual dysfunction.
If long-standing damage has taken place, surgery cannot always be the means of repairing it. CES is a chronic condition. New ways need to be learned to adapt to body function changes. Physical as well as emotional support is critical.
Involving family in care, professionals need to provide support. Based on limitations, help can be sought from social workers, sex therapists, occupation or physiotherapists, and medical practitioners. To avoid problems, you need quick treatment and reliable medical assistance and supervision.