Pancolitis is a type of ulcerative colitis that affects the entire large intestine. It is also known as pan-ulcerative or total colitis or universal colitis. This is a chronic inflammatory bowel disease as it develops over a long period of time. Though there is no definite cure for this chronic condition but there are certain treatment methods that can improve and relieve the symptoms of pancolitis.
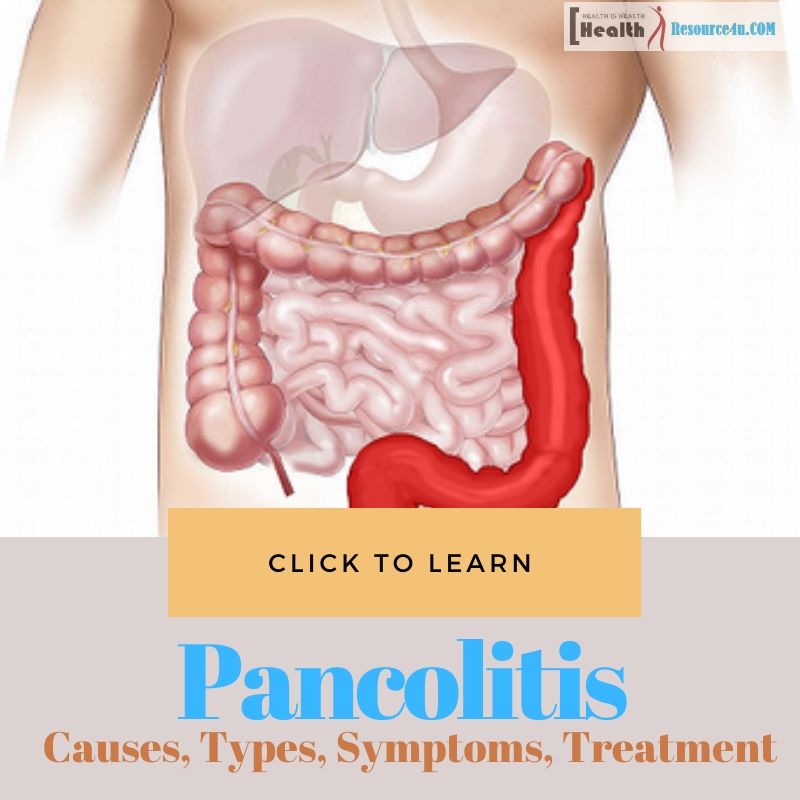
The ulcerative colitis develops long-lasting inflammation and ulcers or sores in your digestive system. It badly affects the innermost lining of the large intestine or colon and rectum which exists at the end of the colon and stores feces before it releases from the body.
The ulcers that develop on colon due to ulcerative colitis disease produce pus and mucus leading to a different kind of abdominal discomfort, rectal bleeding and diarrhea occur.
As per one study report approx, 20 percent of total ulcerative colitis patients develop the pancolitis disease. This major health condition can sometimes lead to life-threatening complications if appropriate treatment is not provided on time to the patient.
Though there is no definite cure for this inflammatory health condition still treatment can improves and reduce its symptoms to a great extent and even deliver remission for a long period of time.
So as soon as someone notices the symptoms of this chronic health condition it is crucial to immediately take the medical help and attention to cope up with this inflammatory condition in a much comfortable way.
Causes
Table of Contents
Though the exact causes of ulcerative colitis are still unknown but scientists believe that there are several influencing factors that cause to develop this inflammatory bowel disease or IBD.
Previously it used to be believed that it is your diet and stress level that triggers the growth of this chronic health condition but later on doctors denied this belief simply. As per the health specialists, your diet and stress level has the ability to aggravate this health condition but these factors themselves cannot cause this chronic bowel disease.
The autoimmune condition is the most common cause considered responsible for ulcerative colitis. In such a condition, your immunity system, instead of fighting or protecting your body from viruses and bacterium invading, fights off your healthy tissues.
As a result of the immune system malfunction your immune system of the body attacks itself to the healthy cells in your digestive tract and develops the signs and symptoms of ulcerative colitis. Apart from this heredity or gene play a vital role in causing this inflammatory bowel disease.
People who have a family history of ulcerative colitis, which means their immediate parents or grand-parents or a close relative are affected with this health issue are more likely to develop this condition with a comparison to those who do not have a family history of this disease.
This condition or factor is also known as genetic predisposition. However, most of the ulcerative colitis patients do not have a family history of this health issue.
Apart from this, an unusual or abnormal response from the digestive system to bacteria existing in the intestine can also cause this inflammatory disease. Sometimes unknown triggers like stress, diet, bacteria, and viruses can cause this bowel disease.
The ulcerative colitis can develop to anyone at any point in time of life. However, it is more common in people aging between 15 to 25 years old including both the genders in equal amounts.
Types of Ulcerative Colitis
Ulcerative Colitis is divided into the following types or forms depending upon its area or location of growth in your body.
Pancolitis
Pancolitis is a severe form of ulcerative colitis which affects the entire colon area. People who develop this health condition notice symptoms like belly cramps, pain, fatigue, severe bouts of bloody diarrhea and excessive weight loss.
Acute Severe Ulcerative Colitis
This type of ulcerative colitis is a rare condition. However when it develops it affects your entire colon area leading to intense pain, fever, heavy diarrhea and bleeding.
Proctosigmoiditis
This type of ulcerative colitis develops in the rectum and lower end of the colon. It is also called the sigmoid colon. People who develop this condition notice symptom like bloody diarrhea, pain and belly cramps. The affected person gets the urge to poop but unable to do so because of severe cramp and pain. Doctors call this condition tenesmus.
Ulcerative Proctitis
This type of ulcerative colitis develops only in your rectum. It is generally the mildest form of UC and develops only a single symptom that is rectal bleeding most usually.
Left-Sided Colitis
The Left-Sided Colitis causes cramps on the left side of your belly. In this case, the inflammation lies between your rectum area to the left side of the colon. In this case, the affected person notices symptoms like bloody diarrhea and unwanted weight loss without any effort towards it.
Symptoms of Pancolitis
The symptoms of pancolitis will vary from person to person. However overall the symptoms of this inflammatory disease are following-
The primary symptoms of pancolitis include
- Frequent diarrhea issue that contains pus, mucus, and blood.
- Urgent necessity or feeling of emptying bowels which cannot be controlled.
- Pain and cramps in the abdominal area are very common phenomena.
The special or typical symptoms of pancolitis include
- Tenesmus is a condition in which you feel the necessity to pass stools in spite of the emptiness.
- Severe weight loss without trying.
- Frequent fatigue and extreme tiredness in the body.
- Fever with body cramp.
- Loss of appetite.
- Night sweats issue when your body sweats excessively at night even though there are cold weather and airflow in the surrounding.
Flare-Ups
Flare-up is a condition in which a pancolitis patient doesn’t experience its symptoms for a significant period and suddenly the symptoms started to appear or return. During the flare-up period, an affected person notices the symptoms in other areas of the body such as-
- Ulcers in mouth
- Pain and swelling in joints
- Red, swollen and painful skin
- Breathing shortness.
- Fast and irregular heartbeat
- Redness and irritation in eyes
- Bloody stools
- Frequent high body temperature
Diagnosing Pancolitis Disease
Your doctor will recommend the following diagnostic or lab tests to confirm the existence of UC or you have developed some other gut health disease.
- Blood Test- The blood test report will confirm whether you have developed inflammation or anemia.
- Stools Test- In this particular diagnostic test your stool will be taken as a sample for the lab test. This test report will help the healthcare specialists to identify whether there is any parasite in your colon or an infection. This test will also help in identifying whether your stool contains blood trace or not which your eyes cannot see.
- Flexible Sigmoidoscopy- In this particular diagnostic test, the doctor will look at the lower area of your colon. For this, they will insert a bendable tube into the lower colon through the bottom side.
This tube has a small light and camera on its surface which will help to see clearly the inside portion. Also, the doctor may take a small piece from the lining of the lower colon through a small tool. This process is known as a biopsy. The tissue sample collected out of this procedure is then sent for the lab test to check under a microscope to rule out any issue if it is there.
- Colonoscopy- This diagnosis process is very much similar to the Flexible Sigmoidoscopy diagnostic procedure. The only difference is that in this process the doctor will look to your entire colon region not only the lower area of the colon.
- X-rays- Though x-rays are the least recommended form of the diagnostic test to rule out this health condition, still under special circumstances or cases your doctor may ask you to have the one.
Treatment
The treatment procedure of pancolitis will depend on the severity of your condition and to the extent its symptoms have affected the lives of its patients.
Though there is no definite cure for treating this disease the aim of its treatment are lies around reducing its symptoms until they vanish. This technique is called remission and then the aim remains to maintain this remission. The two common treatment methods which are in use currently for the treatment of this health issue include medications and surgery which are described below.
Medication
For the treatment of pancolitis following four primary medications are given to the patient.
Immunomodulators
This medication is given for reducing the activity or negative impact of the immune system. It is usually taken as a tablet form for the treatment of a mild or moderate form of flare-ups. However, the consumption of this medicine can make its patient prone to anemia and infections.
Corticosteroids
This medication is prescribed to patients for reducing inflammation in the body. One can consume this medication orally or as a suppository in the rectum or via an enema. This medication is not meant for the long term treatment process as it can develop adverse impacts on your health such as conditions like cataracts and osteoporosis.
Aminosalicylates (ASAs)
This medication is again prescribed for reducing inflammation that leads to pancolitis. It can be taken orally as a capsule or tablet, as a suppository in the rectum or via an enema. This medication is prescribed for the treatment of mild or moderate pancolitis. It hardly develops any side effects.
Biologics
This medication targets certain specific components of the immune system which are involved in inflammation. It is taken via an intravenous infusion or injection.
Surgery
If the prescribed medications fail in improving the condition of pancolitis patients or the flare-ups are causing serious impacts on the lifestyle of the patient then surgery is the only treatment option recommended by the doctors. If surgery performed then the entire colon is removed to ensure that there would be no risk of any form of recurrent ulcerative colitis.
However, before stepping up for surgery, one should have full awareness about its negative consequences risks. This is because once the colon is removed the waste removal is done via a hole in the abdominal area. The waste passes to a special kind of bag known as an ileostomy.
A second surgery may be performed after some time in order to create an internal pouch known as the ileoanal pouch. This pouch establishes a connection between the small intestine and anus so that stools can pass normally like before.
Incorporate Certain Lifestyle Changes
Incorporate the following lifestyle changes in your day to day life which helps in relieving the symptoms of this disease and also helps in avoiding triggers so that it won’t recur.
- Avoid the intake of carbonated drinks.
- Eat the lesser amount of dairy products.
- Reduce the consumption of insoluble fiber.
- Drink plenty amount of water every day, at least 8 glasses of water or 64 ounces.
- Consume multivitamins.
- Maintain a food journal and note down all the foods that you need to avoid for relieving your symptoms.
These vital changes in your diet routine will ensure that your body can easily avail of the necessary level of nutrient keeping all the triggering diet factors aside.
Ulcerative Colitis Complications
Ulcerative colitis contains following complications risks-
- Inflammation- It can affect your joints, eyes and skin area.
- Bleeding- The bleeding caused by this health issue can lead to anemia.
- Dehydration- the persistent symptoms of this disease can lead to dehydration conditions in the body. Hence the patient requires to take fluid through IV if your large intestine is unable to absorb enough amount.
- Osteoporosis- In this condition, the bones get weaker either because of your diet intake or due to the intake of corticosteroids in excessive amounts.
- Liver Disease- In this condition your liver or bile ducts can get inflamed or you may develop scar tissue in your liver.
- Fulminant Colitis- Under the condition of severe UC attack the colon might burst or the infection may spread through your body. The intestine stops moving waste and swelling occurs in your belly.
- Colon Cancer- The cases where UC has affected your whole large intestine or if UC is persistent for longer duration then it increases your risk of developing colon cancer.
For avoiding these major complications risk for your health it is crucial that you pay attention to your symptoms of pancolitis and take necessary treatment on time to get back your lost health and maintain a healthy body throughout your life.
[expand title=”View Article Sources“]
- https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
- https://www.medicalnewstoday.com/articles/320064.php#what-are-the-treatment-options
- https://www.healthline.com/health/pancolitis#outlook
- https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/what-is-ulcerative-colitis#1
[/expand]